Betties, let’s face it: our bodies are remarkable. Take the uterus for example. If the human body had ‘wonders of the world,’ the organ responsible for menstruation, gestation and labor has gotta be a top contender.
And as the uterus finds itself responsible for so many important biological processes, if there’s a malfunction, the ripple effects can result in a host of issues. Today, we’re going to explore one of those conditions: Endometriosis.
What is endometriosis?
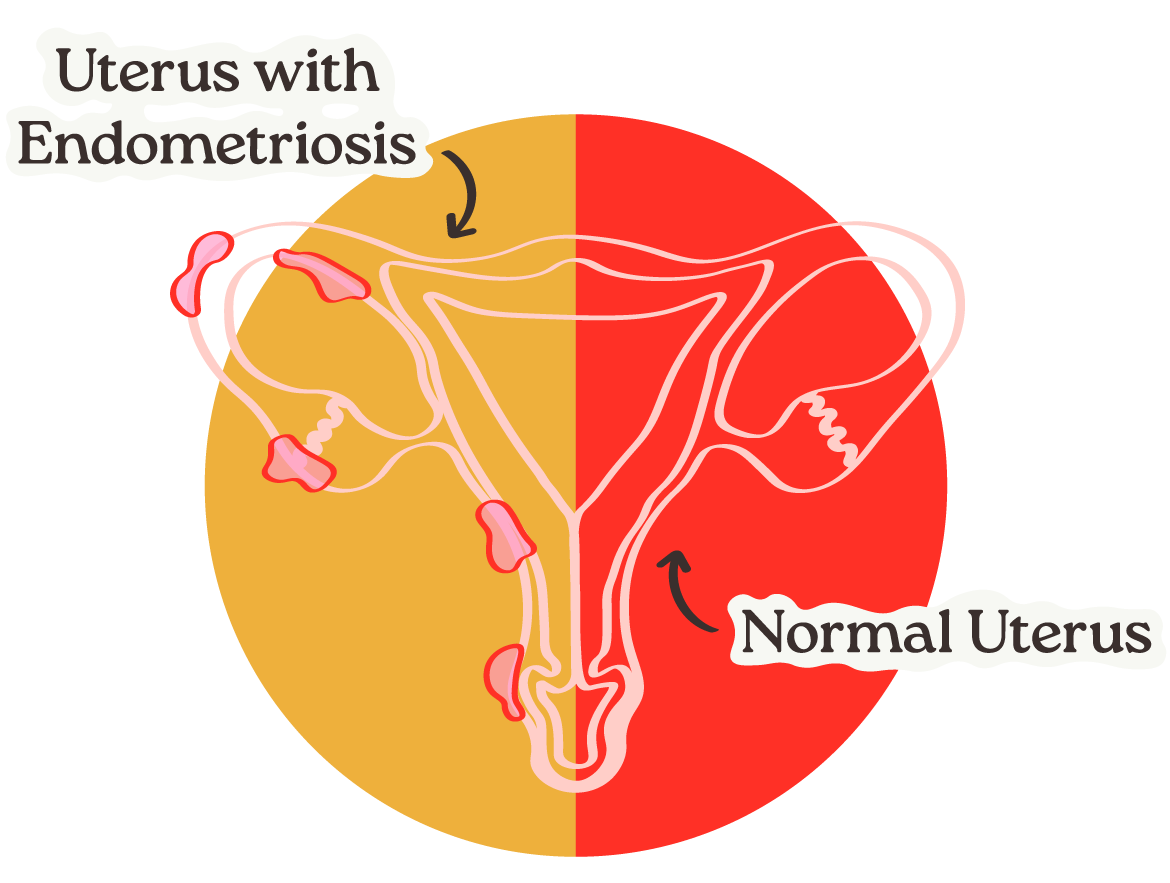
First, a quick rundown on the uterus. The uterus is made of two types of tissue: the myometrium, a really strong thick smooth muscle that contains the endometrium, the complex tissue lining the uterus and responsible for menstruation.
Every month, a Betty’s uterus goes through a series of changes, one of which is a thickening of the endometrium and subsequent shedding if no pregnancy is present. However, sometimes this endometrial tissue can grow outside of the uterus on other pelvic organs, such as the fallopian tube or the ovaries.
During menstruation, this misplaced tissue mimics correctly-placed tissue, responding to hormonal changes which cause the cells to grow, break down and then bleed. However, unlike menstrual blood, blood from these endometrial-like cells has nowhere to go, causing inflammation and scar tissue. And because a Betty’s cycle is, well, a cycle, endometrial tissue continues to develop, resulting in a chronic condition that’s known as endometriosis.
What does endometriosis look/feel like?
When endometrial tissue goes rogue and begins growing where it doesn’t belong, the effects can be debilitating. Often, Betties will experience cramping, sharp or throbbing pain and pelvic pressure 1-2 days before their cycle with pain extending days after their cycle ends. Pain during sex and bowel movements are also possible symptoms.
However, some Betties experience no symptoms at all, stumbling onto endometriosis only when large, complex cysts are discovered on the ovaries or when they have trouble getting pregnant.
Endometriosis implants can cause scarring in the pelvis, including the fallopian tubes, blocking the sperm from reaching an egg, resulting in infertility.
What causes endometriosis?
Betties, it’s a real headscratcher. The cause of endometriosis is not well-understood. However, a few factors have been associated with endometriosis.
· Having a first-degree relative with endometriosis, such as a mother, aunt or sister
· Having a child for the first time after 30 years old
· Low BMI
· Heavy periods lasting beyond 7 days
· Reproductive tract disorders
Because the definitive cause of endometriosis is unknown, diagnosing it can be equally challenging, yet diagnosing it early can be critical in mitigating chronic symptoms. Here are some ways endometriosis is detected:
Track: Keep tabs on your cycle and symptoms to review with your doctor! Looping in your provider about any pain sooner rather than later is important.
Feel: With a pelvic exam, your provider can feel for abnormalities, such as cysts or physical indicators that suggest pelvic scarring.
See: Ultrasounds, MRIs and even a view inside the abdomen through minimally invasive surgery called a laparoscopy may be helpful or even necessary to confirm an endometriosis diagnosis, but not necessary to begin treatment and relieve symptoms ASAP.
How do you treat endometriosis?
Because endometriosis is a condition with no well-understood cause, there is no cure. Treatment is instead focused on the symptoms to stop out-of-bounds endometrial tissue from thickening and breaking down with each menstrual cycle. Some options include:
Hormones
Common forms of contraception, such as combination birth control pills, progesterone birth control pills (aka mini-pills), or Depo-Provera shots, can all effectively suppress the cyclical changes in hormones that cause the endometrium to grow and shed. These contraception methods make for a great one-two punch if you’re looking to prevent pregnancy and seek pain relief!
Pain medication
Adding an NSAID medication (such as ibuprofen) before and during your cycle can give a Betty a break from endo-related pains. Other medications are available – ones that work directly on the hormone pathways from the brain. These can have more side effects but are an option if needed!
Laproscopic surgery
In certain cases, this minimally invasive surgery can help relieve pain and treatment of endometriosis by removing lesions or scar tissue.
Up to 15 percent of all reproductive-aged women live with endometriosis, yet underfunded research and stigmas surrounding this “invisible pain” delay Betties being diagnosed, prevent Betties from finding relief/preserving fertility, and ultimately, hinder the discovery of an endometriosis cure.
Every year, Endometriosis Awareness month gives the mic to those living with it and keeps those charged with funding endo researching accountable. Here at Betty’s Co., when we talk about normalizing women’s health, endometriosis, painful periods, heavy periods are prime examples of the conversations we want to normalize for Betties so they can be their fullest, healthiest selves.
![]()
Have a question about your cycle or symptoms?
Book a Care Close-By appointment!
Betty’s providers are ready to listen to your concerns and can physically assess you to land a diagnosis + a care plan moving forward.







Join the conversation